The recovering addict helping to save lives in Oakland County’s overdose crisis
Paul Shankin turned his life around to save himself from drug addiction — and help others do the same


Audio By Carbonatix
[
{
"name": "GPT - Leaderboard - Inline - Content",
"component": "35519556",
"insertPoint": "5th",
"startingPoint": "3",
"requiredCountToDisplay": "3",
"maxInsertions": 100,
"adList": [
{
"adPreset": "LeaderboardInline"
}
]
}
]
On June 8, 2023, the Oakland County Sheriff’s Office (OCSO) posted a message on social media saying that it had responded to an unusually high volume of calls reporting suicide attempts and overdoses in a 48-hour period. “Many people are facing great personal challenges and there is help available,” the post read.
The message came amid a growing crisis of overdose and drug-related deaths. In Oakland County alone, there was a 68% rise in overdose deaths from 2019 to 2021. In response, OCSO created a crisis response unit tasked with answering drug-related calls, conducting follow-up visits, and providing referrals to recovery and support services in 2022. It was one of the first police agencies in Michigan to do so.
Documents obtained by Metro Times through a Freedom of Information Act request revealed that a single officer followed up on all three of the overdose calls that weekend. Deputy Kyle Hayes of the crisis response unit visited each overdose victim the next day to see how they were feeling, and to offer referrals to support services. He took no action to investigate or arrest any of the people he came into contact with; he was there to keep them from dying and to nudge them toward recovery.
In 48 hours we have responded to multiple suicides, suicide attempts, and saved multiple people who had overdosed. Many are facing great personal challenges.There is help available. Let's continue to share the resources available.The national mental health hotline number is 988.
— Oakland County Sheriff’s Office (@oaklandsheriff) June 8, 2023
He also referred drug users to people like Paul Shankin — a recovering drug addict who now works to inspire others suffering from substance use disorder into finding their own pathway to recovery. He refers to himself as a “peer navigator.”
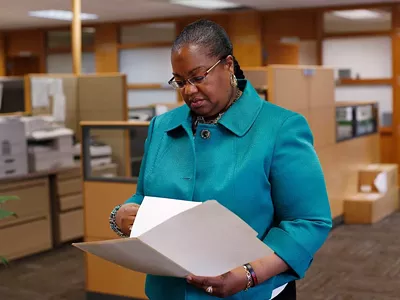
Shankin works at Alliance of Coalitions for Healthy Communities, a prevention, harm reduction, and recovery support network in Oakland County with a goal to combat the increase in co-occurring mental health and substance use problems in the county. The organization also tackles post-overdose calls with its group of trained peer navigators, like Shankin.
People like Shankin have never been more necessary. For years, illicit drug use across the United States has steadily been on the rise. No longer just an opioid epidemic, the drug epidemic has centralized around two categories of substances: synthetic stimulants and synthetic opioids. Of these, methamphetamine and fentanyl are responsible for a growing majority of deaths and overdoses.
The surge has sparked a shift in the way communities are addressing the crisis. Diverging from strict abstinence, many organizations are adopting a harm reduction approach, focused on keeping users alive. Shankin’s journey — from the reasons for his addiction, to his response and recovery — all mirror this shift, reflecting larger trends in America’s drug crisis.
Reason
Shankin was born in 1981 and grew up in a white, lower-middle class family in Warren, in a neighborhood which today he describes as being “just infested with narcotics.” His father, a roofer, and mother, a homemaker, both regularly used, exposing him to substance abuse at a very early age. “I knew what alcohol was, I knew what drugs were, when I was in elementary school,” says Shankin.
The summer before he entered sixth grade, Shankin graduated from the D.A.R.E program. That same summer, he started experimenting with alcohol and marjuana. Shankin was 11.
At home, both substance abuse and mental health issues were prevalent. According to the Substance Abuse and Mental Health Services Administration, one in four adults with serious mental illness turn to illicit drugs.
Over time Shankin says he developed borderline personality disorder, and that the scope and scale of his use expanded. “All through high school, I was using narcotics,” says Shankin. He began experimenting with all different kinds of controlled substances: psychedelics like mushrooms, LSD, mescaline, and ecstasy. Then he graduated to prescription pills.
This use continued after he turned 20 in 2001, paralleling the dawn of the opioid epidemic in the United States.
In the late 1990s, pharmaceutical companies began to aggressively market prescription opioids as non-addictive, leading doctors to massively overprescribe opioid painkillers like OxyContin. Prescription pills gave way to widespread misuse and addiction among users, who turned to heroin in the 2010s, and later synthetic opioids like fentanyl.
The first time Shankin saw OxyContin was when a friend, recently discharged from the U.S. Marine Corps, was prescribed 80 milligrams of the drug to treat an injury from basic training. “He just had, like, bottles of it,” says Shankin. “He introduced that to me somehow, and I eventually got hooked.”
“I got out of jail, and then not even 24 hours, I was getting high,” says Shankin. “I just remembered how powerless and just distraught — I couldn’t believe everything that I had built up within myself to not use just vanished.”
tweet this
Shankin began seeking drugs in doctor’s offices, feigning symptoms in return for diagnoses and prescriptions. He had learned how to communicate with doctors to get any medication he desired. When he wanted to try Adderall, he Googled “why people take Adderall” and studied the symptoms of attention deficit disorder.
“I had gone into a place and just acted,” Shankin says. “Like, ‘This is what happens to me when I’m at home, I can’t keep my attention for more than five minutes,’ and just play completely dumb to the whole system.”
Shankin was part of a greater trend in overprescription. This was before Michigan’s Automated Prescription System, a tool used by prescribers and dispensers to track controlled substances, assess patient risk, and combat prescription abuse and diversion at the prescriber, pharmacy, and patient levels. This is why pharmacists ask for a patient’s ID when dispensing controlled substances.
“So I was part of that whole problem in the beginning,” says Shankin.
Shankin quickly became dependent, trading OxyContin for heroin when the cost of prescriptions became too much.
Heroin is a semi-synthetic opioid synthesized from morphine. Used for its euphoric and pain-relieving effects, it can be injected, smoked, sniffed, or snorted. The drug is powerful, both physically and psychologically addictive, and carries a high risk of overdose and death. However, according to the National Institute on Drug Abuse, heroin deaths have been decreasing in recent years, with 13,165 deaths reported in 2020, 9,173 in 2021, and 5,871 in 2022.
That is likely because today, heroin is being replaced by fentanyl and other synthetic opioids in most drug markets. As a pharmaceutical it is administered as both an anesthetic and a painkiller. When removed from its medical setting, it is highly addictive in part because it comes so concentrated. Ounce for ounce, fentanyl is 50 times more powerful than pure heroin. It is also cheap and easy to produce. The white power can be sold alone, mixed with other drugs, or stamped into pills mimicing prescription medications.
The New York Times reports that fentanyl is lowering life expectancy in the U.S. and becoming a leading cause of death in recent years. In 2021 alone, fentanyl was responsible for 108,000 deaths, according to the Centers for Disease Control and Prevention.
By the time he entered his thirties, Shankin had tried cocaine, methamphetamines, heroin, fentanyl, ecstasy, molly, psilocybin mushrooms, LSD, marijuana, alcohol, mescaline, angel dust, Xanax, Adderall, OxyContin, Opana, Percocet, Vicodin, Norco, Valium, and Klonopin. But he settled into using crack cocaine and methamphetamine. “I was Stimulant Guy,” said Shankin. “I always liked drugs that got me up.”
For Shankin, 2016 was a blur. He doesn’t remember when or in what order many of the following events happened. But by the end of the year, his wife filed for divorce and his younger sister had died of a fentanyl overdose. He was also homeless, sleeping on friend’s couches, and in abandoned houses around Seven Mile and Gratiot. At times he was sleeping outside. “It was just one of them cycles of where I knew I was really strung out,” he says.
Then he overdosed.

Response
When he overdosed, Shankin had just checked into the detox wing of a Meridian Treatment Center in Waterford. He was using fentanyl and prescription valium and smoking crack cocaine. The combination proved severe enough that reviving him required five doses of Narcan: three nasal sprays at the center, and two injections later on at Pontiac Central Hospital.
But the shock to his system was no match for the draw of the drugs. “I ended up walking out of treatment, like, two days later and was getting high again,” says Shankin.
Countless times, Shankin attempted treatment through standard five-day detox programs at facilities like Sacred Heart in Richmond and Meridian in Waterford. Most of these programs are designed to safely get substances out of a patient’s system, prior to inpatient treatment. They aim to get patients as healthy as possible before their discharge date, but users often forgo follow-up treatment and, without the proper support and coping mechanisms, end up using again.
Shankin says people put too much faith in these treatment programs. “If you’re strung out on some drugs,” he says, many people think that “all you got to do is go to a treatment center and then get off of the drugs, and that’s going to fix everything.” He continues, “That’s the misconception of it — that it’s like a fix-all package.”
As part of his treatment, Shankin was prescribed Suboxone, a medication used to treat opioid dependency. But he even started abusing that.
Medication-assisted treatments like Suboxone and methadone target the brain’s opioid receptors, allowing users to function without opioids. However, the drugs used in medication-assisted treatment only work for opioids. They are virtually useless on stimulants.
Shankin was on a variety of substances when he overdosed. He described taking heroin to come down from days high on crack cocaine, only the heroin was actually fentanyl.
In this way, too, Shankin was part of a concerning trend. Laced drugs and polysubstance use are making substance abuse less treatable and more deadly. Speedballs, or goofballs, are mixtures of heroin or fentanyl and methamphetamine. The intention is to offset the drowsy effects of opioids with the “fireworks” of meth. According to the CDC, in 42% of opioid overdoses there is a stimulant present. So Shankin was walking a dangerous line.
Soon after, Shankin was arrested and sent to jail for possession of a controlled substance.
The whole time he was in jail, he was determined to stop using. In addition to his sister’s death and the divorce, he felt like had not seen his kids “in forever.” In his cell, he told himself again and again: “I’m not going to get high, I’m not going to get drugs anymore.” He thought he had reached a turning point.
“And I got out of jail, and then not even 24 hours, I was getting high,” says Shankin. “I just remembered how powerless and just distraught — I couldn’t believe everything that I had built up within myself to not use just vanished.”

Recovery
Eventually, Shankin found sobriety through the Twelve Step program. He has been sober since 2018.
Twelve Step programs like Alcoholics Anonymous, Narcotics Anonymous, and Gamblers Anonymous are rooted in abstinence and fellowship. They function as a support group, encouraging members in their sobriety, and helping them to learn how to live a new life with a new code of behavior.
“There’s just a network of men that took me under their wing and literally just retaught me how to live life from the scratch,” says Shankin. “I mean, all the way from just brushing my teeth and taking a shower every day to eating three times a day, to physical fitness, to getting up early in the morning, going to work.”
This support system empowered Shankin, and he started developing principles to apply to his daily life. “They taught me how to start giving that back to people,” says Shankin. As he regained control of his life, he felt a strong need to help others who were struggling with addiction. That desire led him to his work with Alliance, which in turn helped stabilize him. “It ensures my ability to be able to stay sober,” Shankin says of being a peer navigator. “As long as I do that, I can do this until the day I die.”
Now, Shankin starts his day around 6:30 a.m., attending his daily recovery support meeting. Then he calls work to receive his plan for the day. He spends the next 8 to 12 hours connecting with post-overdose users via call, text, or, if unresponsive, by visiting their homes, going door-to-door with deputies from the Oakland Country’s Crisis Response Unit. His focus: to build rapport and trust with people in high risk situations, and to let them know there is help available.
Fentanyl has made high risk situations more common and fatal, making overdose reversal medications like naloxone crucial to saving lives.
For years, naloxone or Narcan, has been the only available option. In November, Oakland County Sheriff’s Office became the first in the United States to deploy Opvee, a new life-saving intervention for treating overdoses. According to the FDA, Opvee may be more effective in reversing overdoses from synthetic opioids like those from fentanyl.
Reflecting
Shankin’s story has a happy ending: He is a Twelve Step sponsor, a taekwondo teacher, and a father to his children. But for many others, abstinence-based programs like Twelve Step do not work. Shankin knows that the pathway he took to get clean is not always what people need. And it is different from what he does at Alliance.
At Alliance, Shankin is a Harm Reduction and Recovery Support Specialist. Unlike the Twelve Step program, a harm reduction approach does not push abstinence, but instead prioritizes safe drug use. Organizations offer users sterile equipment, tools to check their drugs for the presence of fentanyl, and medication to reverse overdoses, blunt cravings, and ease withdrawal-induced nausea.
Having lived through the journey of addiction and coming out the other side, Shakin understands how it is for people in these high-risk situations. Being a peer navigator is where Shankin marries his experience with his work in harm reduction.
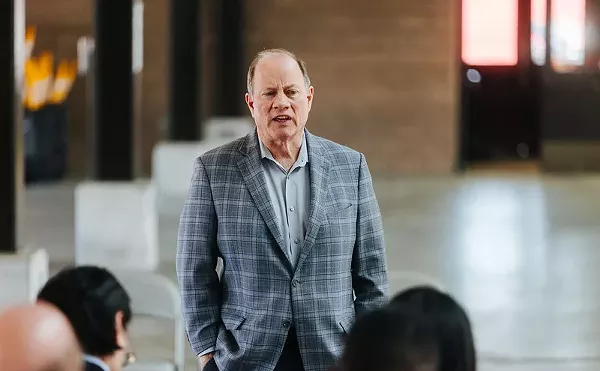
“Peer navigators have a unique language and understanding of what people are going through,” says Steve Norris, Director of Harm Reduction and Recovery Support at Alliance. “They can really approach those situations from a more empathetic and compassionate perspective.”
Reflecting on his experience, Shankin feels there was always part of him that had enough. “I really didn’t want to be doing this. I didn't want to be using, I didn’t want to be living like this, and I did not know how to get out of it,” he says. “But there was nobody there that wanted anything to do with me.” He said that is where the importance of harm reduction comes in: “it doesn’t cancel them out as a human being.”
At its most extreme, harm reduction looks like safe injection facilities, heroin-assisted treatment, and decriminalizing the possession of all drugs, including hard drugs like fentanyl and meth. Radical harm reduction plans have already been rolled out in Oregon and Vancouver, to mixed results.
The shift has not been without controversy. Critics claim the harm reduction approach enables drug users, while supporters claim it keeps users alive while providing them with access to treatment and support. In March, the governor of Nebraska vetoed a bill that would have legalized needle exchanges in the state.
But supporters have good reason: as drugs are becoming more fatal, they argue, keeping people alive is more important than ever. In 2021, Joe Biden became the first president to endorse harm reduction.
Oakland County is far from the Vancouver model. But it has acknowledged that the old approach isn’t working. In addition to the Crisis Response Unit at OCSO and partnerships with organizations like Alliance, they have together established a fatality review board, used to catalog and analyze every overdose death. The board follows each life, from birth to death, identifying what the issues were, where public health corrections failed, and how we can do better as a county.
For Shankin’s part, harm reduction is the way forward because for the first time users are “not being shamed from the jump.”
“To not judge them, but to be with them and also hold them accountable where they’re at, has been something that has been pretty awesome to witness.” says Norris.
“They got the support that’s literally being brought right to their front door,” says Shankin, “It’s pretty powerful.”