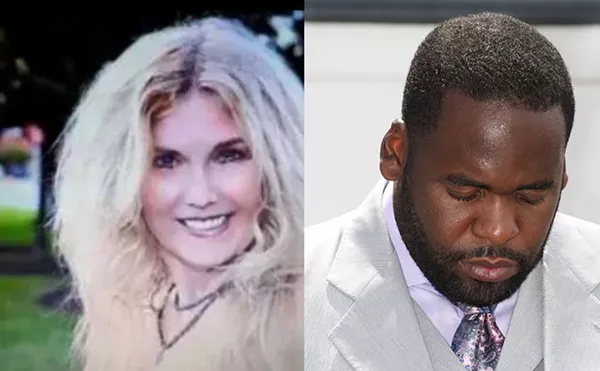
Not many women feel like Dearborn resident Colette Simkins felt immediately after giving birth.
"I wanted to party," exults the 37-year-old mother of seven. "I felt fabulous."
The arrival of seventh child Ellen Margaret last July was a radical departure from the "horrible experience" of delivering her first child in a local hospital 15 years ago.
Ellen Margaret was delivered by a midwife into a water-filled kiddie pool in Simkins' own living room, surrounded by friends and family members.
It was a relaxed atmosphere. Perfumed candles burned in the room, and Simkins listened to a Keith Green CD during labor. During contractions, she sang choruses from a favorite church hymn.
"My midwife helped me walk when I needed to, and let me shower when I wanted to do that. She brought me tea, massaged my back, rubbed my feet, and put a cool compress on my forehead," says Simkins.
The midwife focused her attention on Simkins' every need, helping her through Ellen Margaret's birth.
"It was wonderful," says Simkins. "My midwife was with me spiritually, mentally and physically."
Such a scene might seem unusual in the late 20th century, when the majority of American women rely on doctors and hospitals to deliver their babies. But increasingly, women such as Simkins are challenging modern labor and delivery practices, and turning to midwives for prenatal, delivery and postpartum care.
A recent Centers for Disease Control (CDC) study shows that in 1995, 6 percent of all U.S. births were delivered by certified nurse-midwives, twice as many as in 1989. In Michigan, some 5 percent of all births were attended by nurse-midwives in 1994.
"In the early 20th century, as the medical profession was becoming more organized, doctors called for the outright elimination of the midwife," says Geradine Simkins, a certified nurse-midwife who has practiced in Traverse City since 1976 (and is Colette Simkins' sister-in-law).
"Due to the strong and organized American Medical Association lobby, midwifery in America was almost wiped out," she says. "The influence of women healers and midwives came to a virtual end in the early part of the 20th century."
But now, as Americans begin to re-embrace natural health care practices, there is more demand for such woman-centered care.
Colette Simkins says she values modern medicine, but also believes that in some cases natural nurturing is the best solution -- especially when there isn't a problem.
"Doctors often treat birth as a sickness, and it's not. I know women and babies can die, and I'm not saying we should go back to the Middle Ages, but women can have a birth experience at home without medical intervention," she says. After her first two children were born in hospitals, she used midwives to deliver her last five babies because "they are so attentive to you."
Like doctors, midwives begin patient care during pregnancy. They spend a lot of time talking with each client, and also address nonphysical concerns, such as sexuality and family relationships.
Midwives pride themselves on listening to women, and say they provide support for the body, mind and soul. After the baby is born, midwives may also help with breast-feeding and offer well-baby care.
Before labor, a midwife helps her client fashion a "birth plan," a list of preferences which can include whether a woman wants to walk during labor, if she'll receive liquids, how often she'll be monitored if she's in a hospital, and even if she wants an episiotomy. Postpartum options include putting the baby immediately to breast and keeping the mother and child together in the same room.
For a home birth, the plan may include the name and phone number of a nearby doctor, and the quickest route to the local hospital. Well-trained midwives recognize signs of distress, and don't hesitate to call for physician intervention.
While Colette Simkins chose to have Ellen Margaret at home, many women opt to deliver their babies in hospitals, attended by midwives instead of doctors.
Midwife Sally Simpkins (no relation) is a certified nurse midwife at Sterling Women's Medical Center in Sterling Heights, a clinic which employs three nurse-midwives and a physician and boasts some 11,000 patients. Simpkins and her colleagues deliver babies at area hospitals and will call in the doctor if a complication arises.
In most midwife-assisted births, however, doctors are unnecessary. Recent findings by the Public Citizen's Health Research Group show that midwife clients are less likely to have Caesarean sections or episiotomies. And, according to the CDC, birth outcomes for midwives are also better, with the risk of infant death nearly 20 percent lower for births attended by certified nurse-midwives than for births attended by physicians.
The CDC suggests midwife success is due partly to better prenatal, labor and delivery care practices, and more time spent with patients, both at prenatal visits and throughout labor and delivery. As a result, women are more relaxed.
"Women feel comfortable talking to women," acknowledges Simpkins.
Women who use midwives are uniformly enthusiastic about their experiences. Karen Troshynski-Thomas, 31, was assisted by a midwife during the birth of her first child, Jack, last year at Royal Oak's Beaumont Hospital.
"I had talked to other women, including those who had bad birth experiences. I did a lot of reading on midwifery, and discovered that their take on things was that having a baby was a normal part of life," says Thomas.
She most enjoyed her midwife's laid-back attitude, which allowed her to remain at home all day during labor. Thomas arrived at the hospital at 9:45 p.m., and Jack was born shortly before midnight.
"Using a midwife was more personal. Our labor and delivery was centered on my husband and myself. Our midwife helped us through the end part, the rough part. She was very supportive," Thomas recalls.
Perhaps the only group unenthusiastic about the growth in midwifery are traditional OB-GYNs.
"There is a lot of negativity and hostility toward midwives," says Dr. Brian Mason, an assistant professor of maternal and fetal development at Wayne State University-Hutzel Hospital.
Mason is well-versed in the history of midwifery and, unlike some of his colleagues in the medical establishment, is a strong proponent of midwifery. For the last four years, he has served as physician liaison for midwives at Hutzel, which in 1980 became the first hospital in the state to establish a nurse-midwifery practice.
Mason attributes the hostility partly to increased competition, which makes some doctors see midwives as vying for increasingly smaller slices of the managed health care pie.
"Midwives usually attend to low-risk, easy, no-sweat births. These are wonderful experiences. Everyone is happy and it's one of the most beautiful events in life. The doctors are only called in for the complicated cases, which can be frustrating to some doctors," Mason says. "Sometimes doctors think, 'Don't call me in for the messy part. If you can't do the whole job, then let me do it from the start.'"
Another factor, Mason notes, is a "certain amount of arrogance" among doctors. "Some doctors think that anyone not at your level of training isn't qualified to do the job."
To Mason, the answer is education.
"You would be amazed at what people believe," Mason says. "Midwives are not witches and don't use voodoo."
And midwives are not competition to obstetricians. "They provide something different," says Mason. "And this may appeal to a certain type of patient."
At the same time, he believes some controls are necessary. At Hutzel, for example, there are strict institutional guidelines regarding what midwives can and cannot do. And Mason is currently editing a set of midwife protocols which will be published next year, in response to increasing demand for information from Hutzel from hospitals worldwide. These protocols require midwives to be highly skilled and certified. They can't take on patients with troublesome medical histories, and a doctor is always on call.
"The big risk is that a complication will set in and the midwife isn't prepared," he notes.
Veteran midwife Simkins wouldn't argue with Mason's assessment. "The best of all worlds is a collaborative arrangement between physicians and midwives. Collectively we can offer women the best care," she says.
"I believe that midwives carry both the vision and the skill required to bring forward the best of the old worldview and to forge the new frontiers in women's health care that serves the individual, the family, the community and the world in a wholesome, enriching and sustainable manner."
Types of Midwives
* Traditional or Lay Midwife
Not formally trained, they have learned about birth through personal experience and by helping other women. Sometimes called "granny" midwives. These women attend to home births.
* Direct-Entry Midwife
Has completed a course of training, either in a school or through an apprenticeship. Once she meets requirements for licensing by a state midwifery association, such as the Michigan Midwives Association, she is a CM (Certified Midwife).
Certified Professional Midwife (CPM)
Signifies national certification.
Certified Nurse-Midwife (CNM)
Registered nurses who have passed a national midwifery examination administered by the American College of Nurse-Midwives in Washington, D.C. Some 5,000 CNMs practice across the U.S., with about 150 in Michigan. Most work in clinics or hospitals, and in Michigan receive reimbursement from Medicaid, Blue Cross/Blue Shield and several other private insurance companies.
Glossary courtesy of Geradine Simkins, CNM, MSN.
The Midwives Alliance of North America (MANA) will hold a "Midwifery in the Mainstream" conference Nov. 12-15 in Traverse City. Events are open to the public. For more information call Michigan Midwife Association at 734-332-1588 or e-mail kmulder@pilot.msu.edu